Some of you may remember my earlier blog titled “Part 1: Hugs Not Drugs”. The blog explained that simply hugging someone can boost a range of hormones and chemicals in your body, including oxytocin. A quick synopsis of how oxytocin impacts our body is provided below:
1) Protects our cardiovascular system (Grewen et al. 2003 & 2005).
2) Reduces free radical production and other inflammatory markers lowering the risk for heart attacks.
3) Increases nitric oxide production causing the dilation of blood vessels, which decreases blood pressure, inflammation and plaque build-up.
4) Helps with depression (Scantamburlo, 2007; Arletti and Bertolini, 1987; Andeberg and Uvnas-Moberg, 2000).
5) Helps with decreasing anxiety symptoms (Scantamburlo, 2007; Andeberg and Uvnas-Moberg, 2000).
6) Acts as an anti-stress neuropeptide (Legros, 2001; see figure 1).
7) Reduces the production of cortisol (Ditzen et al. 2009; Taylor, 2006; Heinrichs et al. 2003).
8) Improves sleep quality by decreasing levels of cortisol.
9) Boosts your immune system (Gimpl & Fahrenholz, 2001; Carter, 2014).
10) Lowers pain sensitivity (Dunbar et al. 2012; Mazzuca et al. 2011).
The last blog focused on WHAT oxytocin does. Today’s blog focuses HOW oxytocin works in our body and how it positively impacts our stress response and improves our mental and physical health.
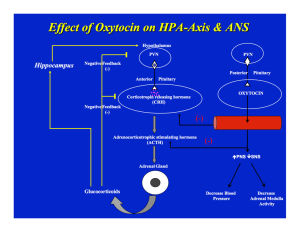
This figure may seem a bit overwhelming, but I promise I will explain every step the best I can. Enjoy!
There are two main pathways in this figure that I will discuss. The first pathway is the stress-response pathway that ultimately leads to the release of cortisol. The second pathway is the oxytocin pathway that leads to the release of oxytocin and is typically activated when you give someone a hug, during intimacy, childbirth and is involved in the milk let-down reflex and social bonding.
The Paraventricular Nucleus (PVN) is located in our hypothalamus (a region of the brain responsible for coordinating and controlling homeostasis). Neurosecretory cells and other neurons, located in the region of the PVN are responsible in releasing neuropeptides and hormones, including oxytocin and Corticotropin releasing hormone (CRH), into the systemic venous and hypopheseal portal system (a collection of blood vessels that connects the hypothalamus to the pituitary). Depending on the situation, one of those two pathways may be it activated.
Let’s start with the stress response pathway. During the stress response, the cells located in the PVN release CRH which then act on cells of the anterior pituitary to release Adrenocorticotrophic Stimulating Hormone (ACTH). ACTH then acts on the adrenal cortex to release cortisol (cortisol is a natural occurring steroid called a glucocorticoid). Cortisol is also known as the stress hormone. Chronic elevation of this hormone can negatively impact our mental and physical health including memory, sleep, depression, metabolism, immune system, wound healing, electrolyte balance, gastric secretion etc.
Now, if you look to the right of this figure (the second pathway) you will see that the PVN also releases oxytocin neuropeptide into the blood stream. Oxytocin is associated with lowering the release of CRH and ACTH (look at the arrows with the red [-] sign). If CRH and ACTH are suppressed, then glucocorticoid (cortisol) production decreases. In addition to acting on the Hypothalamic-Pituitary-Adrenal Axis (HPA Axis), oxytocin acts on the parasympathetic nervous system (PNS) and the sympathetic nervous system response (SNS) which make up our Autonomic Nervous System (ANS). More specifically, it increases the PNS activity and decreases the SNS activity. The PNS is responsible for “resting and digesting,” lowering heart rate and blood pressure. The SNS on the other hand prepares us for “Fight or Flight” by increasing heart rate above 100 beats per minutes, stress response, and shutting down our digestion when signaled. However, with the release of oxytocin the SNS activity is lowered to its original threshold. This can be achieved by a simple hug.
How is this related to mental health:
In individuals with anxiety, the SNS and HPA Axis are often being activated and the release of the stress hormones increase, resulting in the symptoms that many individuals with anxiety experience (i.e., increase in heart rate, dizziness, excessive sweating, sleep difficulties, shortness of breath, increased alertness, excessive worry, restlessness, etc.). Hence, when you activate the oxytocin pathway the activity of the SNS and the HPA decrease, resulting in lowering your stress-response (Carter, 1998; Insel, 1997). Also being able to control the chronic elevation of cortisol can limit memory impairment, sleep difficulties, and depression and can also help with metabolism as well as immune system functioning etc.
*Tips for General Public: remember in order to feel and benefit from the effects of a hug you must hug for at least 20 seconds with each hug. Also the more hugs you give and receive (resulting in repeated exposure of oxytocin release), participation in social bonds might gradually bring about long-term changes in stress reactivity (decrease in SNS and increase in PNS activity) that promote not only psychological feelings of comfort and security, but also cardiovascular health.
*Tips for Mothers: More often than not mothers give their little ones frequent hugs and adequate caregiving, which is important because even a simple hug has many benefits for your child. In contrast, inconsistent caregiving and not providing infants with adequate care has been shown to increase insecure attachment in children, lowering vegal tone, increasing anxiety, depression, anger and stress for the child. So providing consistent caregiving and care is vital for a child’s health. In animal studies, simple maternal touching reduces the entire stress response in children (Pihoker, Owens, Kuhn, Schanberg, & Nemeroff, 1993; Wang, Bartolome, & Schanberg, 1996) so as so continue to give your little ones a hug at least 1-2x per day.
***Note. A hug is not intended to substitute for conventional medicine. If you have been prescribed medication by a physician please follow your physicians recommendation. You can always use a hug as a complimentary method but not as an alternative treatment method to reduce the above mentioned effects.
REFERENCES
1. Andeberg, A.M., Uvnas-Moberg, K., 2000. Plasma oxytocin levels in female fibromyalgia syndrome patients. Z. Rheumatol. 59, 373–379.
2. Arletti, R., Bertolini, A., 1987. Oxytocin acts as an anti-depressant in two animal models of depression. Life Sci. 41, 1725–1730.
3. Bartz, J.A. et al. (2010) Oxytocin selectively improves empathic accuracy. Psychol. Sci. 21, 1426–1428.
4. Carter, C.S. (2014). Oxytocin pathways and the evolution of human behavior. Annu Rev Psychol.
5. Carter, C.S. (1998). Neuroendocrine perspectives on social attachment and love. Psychoneuroendocrinology, 23, 779–818.
6. Ditzen, B. et al. (2009) Intranasal oxytocin increases positive communication and reduces cortisol levels during couple conflict. Biol. Psychiatry 65, 728–731.
7. Dunbar RIM, Baron R, Frangou A, Pearce E, van Leeuwen JC, et al. 2012. Social laughter is correlated with an elevated pain threshold. Proc. R. Soc. B 279:1161–67.
8. Gimpl G, Fahrenholz F. 2001. The oxytocin receptor system: structure, function and regulation. Physiol. Rev. 81:629–83.
9. Grewen, K.M., Anderson, B.J., Girdler, S.S., Light, K.C., 2003. Warm partner contact is related to lower cardiovascular reactivity. Behavioral Medicine 29, 123–130.
10. Grewen, K. M., Girdler, S. S., Amico, J., and Light, K. C. (2005). Effects of partner support on resting oxytocin, cortisol, norepinephrine, and blood pressure before and after warm partner contact. Psychosom. Med. 67: 531–538.
11. Heinrichs, M., Baumgartner, T., Kirschbaum, C., Ehlert, U., 2003. Social support and oxytocin interact to suppress cortisol and subjective responses to psychological stress. Biol. Psychiatry 54, 1389–1398.
12. Hurlemann, R. et al. (2010) Oxytocin enhances amygdala-dependent, socially reinforced learning and emotional empathy in humans. J. Neurosci. 30, 4999–5007.
13. Insel, T.R. (1997). A neurobiological basis of social attachment. American Journal of Psychiatry, 154, 726–735.
14. Legros, J.J., 2001. Inhibitory effect of oxytocin on corticotrope function in humans: are vasopressin and oxytocin ying–yang neurohormones? Psychoneuroendocrinology 26, 649–655.
15. Mazzuca M, Minlebaev M, Shakirzyanova A, Tyzio R, Taccola G, et al. 2011. Newborn analgesia mediated by oxytocin during delivery. Frontiers in Cellular Neuroscience. 5(3); 1-9.
16. Pihoker, C., Owens, M. J., Kuhn, C. M., Schanberg, S. M., & Nemeroff, C. B. (1993). Maternal separation in neonatal rats elicits activation of the hypothalamic-pituitary-adrenocortical axis: A putative role for corticotropin-releasing factor. Psychoneuroendocrinology, 18,485-493.
17. Scantamburlo G, Hansenne M, Fuchs S, Pitchot W, Marechal P, Pequeux C, Ansseau M, Legros JJ. (2007). Plasma oxytocin levels and anxiety in patients with major depression. Psychoneuroendocrinology. 32:407–410.
18. Singer, T. et al. (2008) Effects of oxytocin and prosocial behavior on brain responses to direct and vicariously experienced pain. Emotion 8, 781–791.
19. Taylor, S.E. (2006) Tend and befriend: biobehavioral bases of affiliation under stress. Curr. Dir. Psychol. Sci. 15, 273–277.
20. Wang, S., Bartolome, J. V., & Schanberg, S. M. (1996). Neonatal deprivation of maternal touch may suppress ornithine decarboxylase via downregulation of the proto-oncogenes c-myc and max. Journal of Neuroscience, 16, 83-842.